What To Do If You Are Bitten By A Tick
Tick season is in full-swing. Last week, my son found a tick embedded in his skin after a camping trip. Everyone in my family is well aware of my father’s missed diagnosis and years’ long battle with Lyme disease, and it’s co-infections. Lyme disease has brutalized his health for years. Needless to say, the fear was significant.
The best way to prevent tick borne diseases in the first place is to not get bitten. But that isn’t always possible. So what can you do to protect yourself when faced with a tick bite?
STEP 1 – Take A Picture Of The Tick While The Tick Is Still Attached
This will show details of the tick to identify the type of tick, how deeply embedded the tick is, and how engorged it is.
STEP 2 – Carefully Remove The Tick
It is critical to PROPERLY remove the tick.
- DO NOT squeeze, twist or squash the tick. If you squeeze the tick it may expel more pathogens into your body.
- DO NOT burn it with a match or cover it with Vaseline or oil. This could agitate it to release more pathogens into your system.
- Use a fine-point tweezers to slowly and carefully grasp the tick’s mouth parts by getting as close to the skin as possible.
- DO NOT pull back abruptly; this may tear the tick’s mouth from the body and leave mouthparts embedded in the skin.
- Gently pull the tick straight out with a steady, slow, and even pressure. You must proceed slowly and patiently. Pull steadily without twisting. Try to ease the tick straight out of the skin. It may take several seconds to a few MINUTES for the tick to unhook its mouth. It should release itself from the skin. This can take quite a long time.
- Wash the tick bite area with soap and water. Then disinfect the site with rubbing alcohol. You can then apply a triple antibiotic ointment.
STEP 3 – Identify The Tick And It’s Possible Pathogens
Different kinds of ticks can carry different bacteria, viruses and parasites. Two general families of ticks are found in the United States: Ixodidae (also known as hard ticks) and Argasidae (these are soft ticks). There are only a few ticks within those 700 plus species that are known to bite and transmit disease to humans.
- After removing the tick, place it in a small plastic bag.
- Write your name, date, site of bite and approximately how long the tick was attached on a separate piece of paper and tape to the bag.
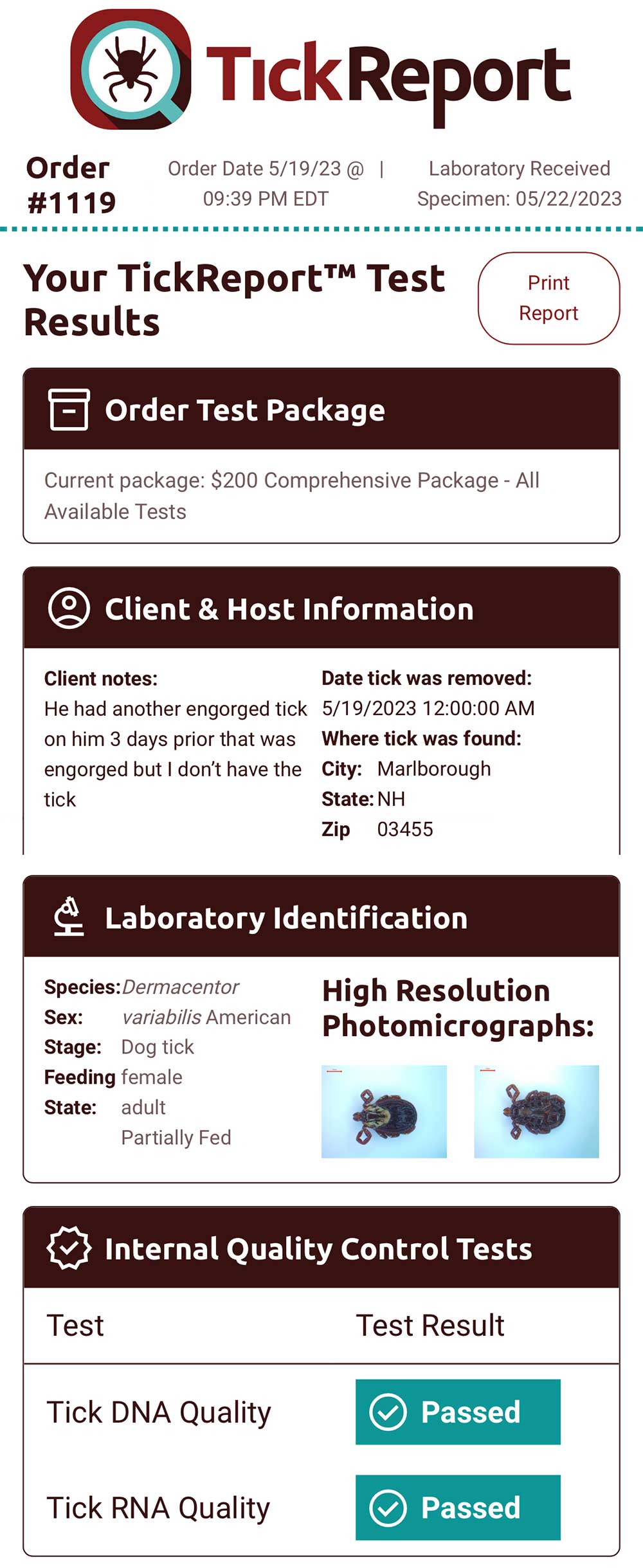
I personally recommend using a company called TickReport to identify the type of tick and pathogens they may carry.
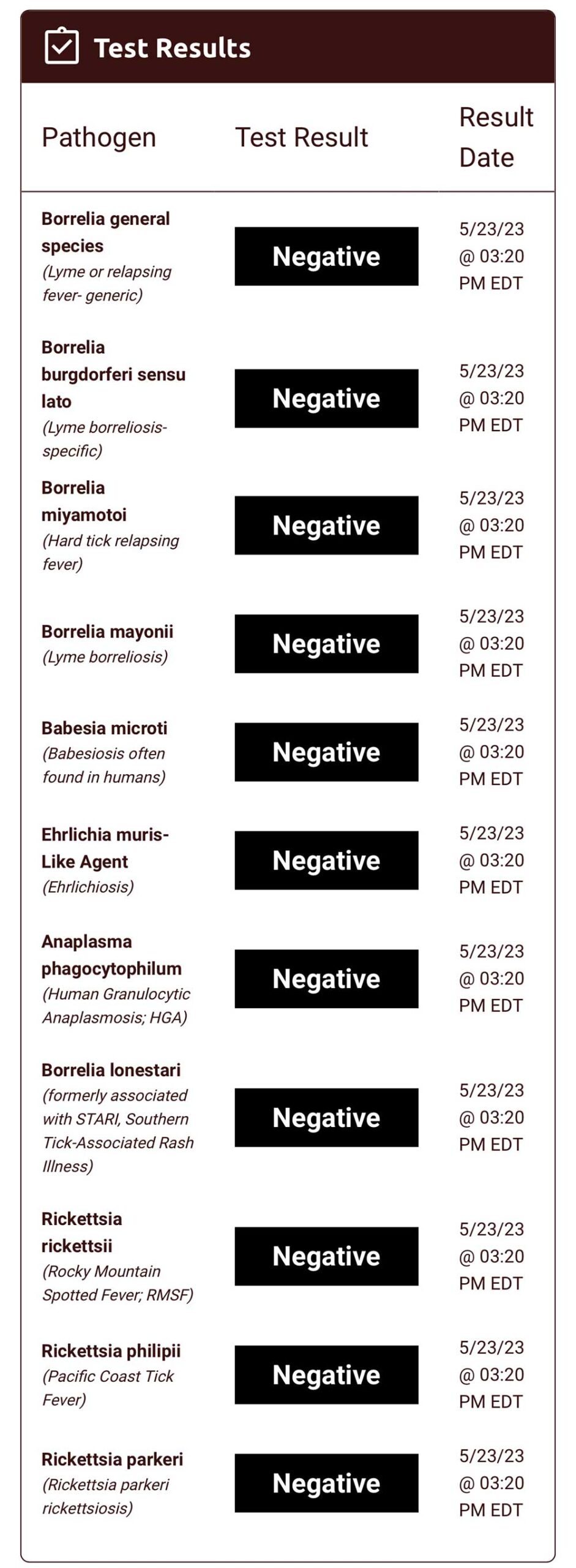
Here is a a copy of my son’s report we got back after submitting the tick by mail. They looked for 23 different pathogens and the turnaround time was about 72 hours.
STEP 4 – Start Tick Bite Treatment
The concerning thing about a tick bite is that it can transmit pathogens in as little as 15 minutes. Although it is clear that the longer a tick is attached, the more likely it is to transfer diseases, no one really knows how long a tick needs to be attached to transmit infection.
You should not assume that there is no risk of contracting a disease if the tick has been attached for less than 24 hours.
Another misconception is that unless you see a rash you cannot develop Lyme disease. Not everyone with Lyme gets a rash. Studies suggest that only 40-60% of Lyme patients will get an erythema migrans rash, and only 20-30% of those will present as the telltale bullseye rash.
What treatment should be started?
A single dose of Doxycycline has been suggested as a strategy to prevent Lyme disease. Unfortunately this is only effective at reducing the tick bite rash. It does not adequately treat any of the known pathogens.
Should I get a blood test for Lyme after I’ve been bitten by a tick?
There is no point in doing a blood test for Lyme disease soon after being bitten by a tick. First, the standard blood test for Lyme is prone to false-negatives, especially in the first 4-6 weeks after a bite. Your body will not yet produce the antibodies that are detected by the standard test.
Additionally, each tick-borne disease requires a different blood test, each test has varying degrees of accuracy. Testing the tick itself can help you know what you’ve been exposed to and is a better strategy for deciding if and what treatment you may require.
What treatment should I begin?
ILADS (the International Lyme and Associated Diseases Society ) recommends that preventive treatment be discussed with anyone who has had a blacklegged tick bite. According to ILADS:
“An appropriate course of antibiotics has been shown to prevent the onset of infection.
ILADS recommends 20 days of doxycycline (provided there are no reasons you cannot take doxycycline). The decision to treat a blacklegged tick bite with antibiotics often depends on where in the country the bite occurred, whether there was evidence that the tick had begun feeding, and the age of the person who was bitten. Based on the available evidence, and provided that it is safe to do so, ILADS recommends a 20-day course of doxycycline.
Patients should also know that although doxycycline can prevent cases of Lyme disease, ticks in some areas carry multiple pathogens, some of which, including Babesia, Powassan virus, and Bartonella, are not responsive to doxycycline. This means a person could contract a tick-borne illness despite receiving antibiotic prophylaxis for their known bite.
ILADS recommends against single-dose doxycycline. Some doctors prescribe a single 200 mg dose of doxycycline for a known bite. However, as discussed in detail in the guidelines, this practice is based on a flawed study that has never been replicated.”
What if your tick report results are positive?
In this case, you will want to stay on the doxycycline treatment. Many ILADS practitioners prescribe 4-6 weeks for early Lyme. Other pathogens if detected will require different treatment regimens and length of treatment.
If the tick test is negative, that doesn’t mean you are fully out of danger. It depends on your exposure and your symptoms. One thing to consider is how long you were exposed to the ticks and whether there could have been another bite that you did not see. Even though one tick is negative, another undetected one could be positive.
STEP 5 – Look Out For Any Unusual Symptoms That Come Up Over The Next Few Weeks
Examples include: flu-like symptoms, headache, fever, ringing in the ears, weird numbness or tingling, facial palsy, nausea, migrating pain, joint swelling, night sweats.
Write down any symptoms that are not normal for you. These can start anywhere from 1-3 days and up until 4-6 weeks after the bite. Check out this symptom checklist. Check the bite site over the next three weeks for any signs of a rash.
The best way to stay healthy is to be prepared. Know what to do. Have a plan. Take the right steps to keeping you and your family healthy this summer!!

If your family spends a lot of time in the woods hiking, mountain biking, fishing, etc., make sure they take preventive measures.
Please Share the Health if you liked what you read!!!
For more information about my wellness programs and my practice, check out my website drsadaty.com. Hey Look! You are already here…
Ready for the legal disclaimer? Information offered here is for educational purposes only and does not constitute medical advice. As with any health recommendations, please contact your doctor to be sure any changes you wish to consider are safe for you!
Thank you Dr Sadaty for sharing your story and the very in lightening information. I’m sure most of us had the wrong information on how to remove a tick. I hope your son is doing well.